What do we need to know about bacteria in order to understand how antibiotic resistance emerges and evolves?
Bacteria are different from viruses
Bacteria are often wrongly blamed for infections caused by viruses, which leads to antibiotics being prescribed for treating viral infections. In fact, antibiotics will not work against viruses because they target only bacteria, and bacteria are very different from viruses.
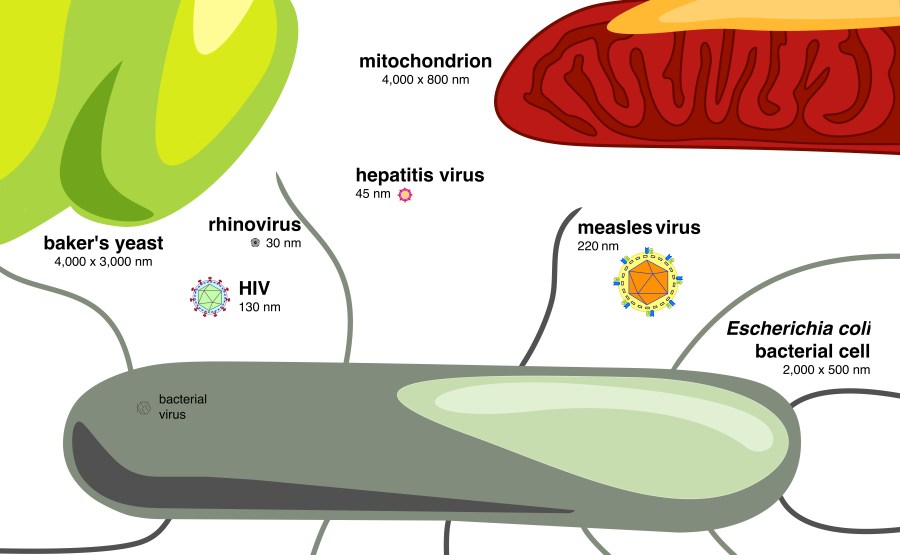
Viruses are the particles that infect organisms such as humans, animals, insects and even bacteria! Viruses are roughly composed of a genome that is encased in a rigid shell. It is the shell surface that recognizes its prey and allows infection to occur. This infection is needed for the virus to multiply.
Bacteria, in contrast, are tiny unicellular organisms that can develop and multiply independently, without infecting host prey. Bacteria are also a lot bigger than most viruses and since they have their own metabolism, their growth can be prevented at many levels with the use of antibiotics. Since viruses are unable to multiply unless they are inside a host, antibiotics will have no effect on the virus itself or on virus multiplication.
What is antibiotic resistance?
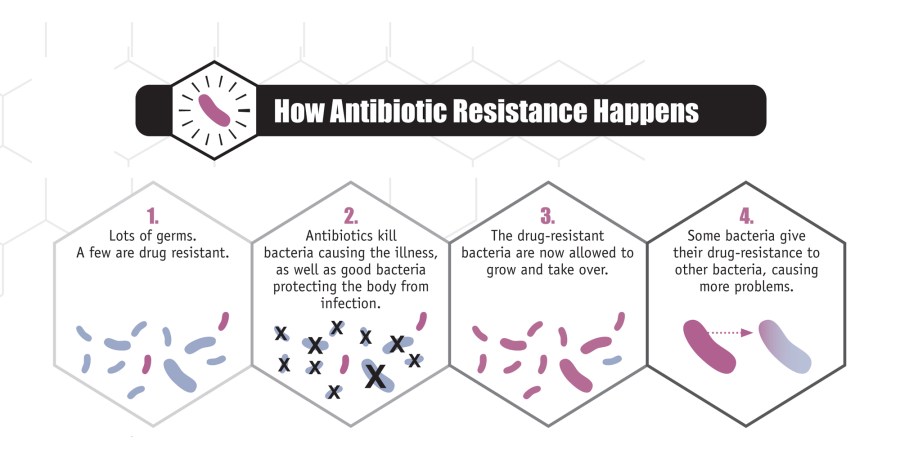
A common misconception is that humans become resistant to antibiotics. It is, in fact, the bacteria, and not the infected human hosts, that become resistant. Antibiotic resistance occurs when an antibiotic has lost its ability to control or kill bacterial growth. In other words, the bacteria will continue growing and multiplying in the presence of therapeutic doses of an antibiotic, and the disease may not be cured.
Why do bacteria become resistant to antibiotics?
Antibiotic resistance is a natural phenomenon. Some bacteria produce antibiotics to eliminate bacterial competitors in their close environment. It is therefore not surprising that bacteria have developed resistance mechanisms to defend themselves against those antibiotics. Antibiotic resistance is ancient and can be found in places where bacteria have had no contact with human life (such as in the deep permafrost for example) or in the gut of remote amazonian tribes.
How do bacteria become resistant to antibiotics?
Bacteria become resistant by acquiring mutations that allow them to survive in the presence of antibiotics. Some mutations eliminate or modify the bacterial structure that the antibiotic attacks whereas other mutations enable the production of chemicals that inactivate antibiotics. Still others shut the gates that allow antibiotics into the cell, and others enable mechanisms that pump the antibiotic back outside, so it never reaches its target. Such mutations usually occur spontaneously but the use of certain classes of antibiotics, especially the ones causing DNA damage, can increase the mutation rate in bacteria.
Another important way by which bacteria can become resistant is through the exchange of genetic information. Bacteria have the ability to swap genes with each other and this is a route by which resistance genes are frequently traded between different types of bacteria. Whether by mutation or genetic exchange, individual bacteria can acquire multiple resistance genes and become resistant against several classes of antibiotics. They are then said to be multi-resistant.
How does antibiotic resistance spread?
Antibiotic resistance traits are inherited by the offspring of resistant bacteria. This means that a resistant bacterium, when it divides, will produce two resistant daughter cells. This is what we call ‘vertical transmission’. As mentioned above, antibiotic resistance genes can also be exchanged between bacteria and this is known as ‘horizontal transmission’. Resistant bacteria can spread anywhere: from person to person, from animal to person (and vice versa), through the air or soil, and in our food and water supplies.

How can antibiotic resistance harm humans?
When humans become infected with antibiotic-resistant bacteria, infections are extremely difficult to treat. Several antibiotics will no longer work and this will allow the infection to spread throughout the body or impact infected tissues. In extreme cases, which are constantly on the rise, there is no medication available for treating the infection. (Read more about gut microbe resistance here and here)
Because bacteria are constantly evolving new ways to counteract or avoid our limited arsenal of weapons, we must 1) prevent the development and spread of antibiotic-resistant bacteria, 2) discover or produce new antibiotics or alternative therapies and 3) educate society about the wise use of these medicines. Find out more about the effects of prolonged antibiotic use.
Why is antibiotic resistance a public health problem?
Because we live in a global society that shares microbes through our increasingly frequent interactions and travels, antibiotic resistance is a growing problem that affects every nation. Independently of how bacteria have acquired their resistance, the overuse of antibiotics is selecting for resistant strains and in many cases promotes the development of resistance. If large numbers of bacteria become resistant, infections will be more difficult to treat, antibiotics will have no effect and the number of deaths due to resistant infections will grow. Read more about the global antibiotic resistance pandemic and our collective responsibility in this situation.
Why is antibiotic resistance an ecological problem?
When humans and animals are treated with antibiotics, approximately 80-90% of the ingested drugs are not broken down but are released as waste into the environment. These antibiotics retain the ability to affect bacteria and can promote antibiotic resistance after they enter the soil or water as a waste product. The fate of new antibiotic-resistant bacteria in the environment remains largely unknown. Find out more about the use of antibiotics as growth promoters in food animals.